Password Reset
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Hip-Spine Syndrome (HiSS), characterized by simultaneous degenerative hip arthritis and lumbar stenosis, represents a condition that is becoming increasingly prevalent as our community ages.1 First identified in 1983 as a difficult condition to diagnose and treat, the correct source of disability was deemed critical to avoid misattributed treatment.2,3 Variations in HiSS are classified in four general categories: simple, complex, secondary, and misdiagnosed. Simple has a clear primary source of symptoms, while complex lacks a definitive primary source. Secondary has both hip and spine pathologies present with interrelated effects of each pathology contributing to the other. Finally, those individuals with misdiagnosed received poorly suited treatment secondary to a misattributed primary pathology.2,4,5
Pain from the lumbar spine, pelvic girdle, and hip overlap as coordinate motion throughout these regions is interrelated. This may present with a structural, kinetic, or physiologic disorder in combined variation. This complex pathology makes for challenging clinical decisions as to which procedures and in what order will provide the greatest benefit.5 Determining the diagnosis, symptom etiology, and correct treatment remains difficult in the management of HiSS.
Although the precise prevalence of coexistent hip and lumbar spine pathologies is unknown, degenerative hip and lumbar pathologies are exceedingly common. In adults over the age of 60, 19% to 47% are estimated to have spinal stenosis,6 and the prevalence of axial spondyloarthrosis and ankylosing spondylitis are estimated to both be 0.35%.7 The hip is among the most common joints to be affected by osteoarthritis (OA) due to its high axial weight-bearing responsibility. Radiographic evidence of hip OA is 27% in patients 45 years of age and older, and the rate of symptomatic hip OA is 9%.8,9
Patients with either hip or spine pathologies can have referred pain to the low back, gluteal, groin, thigh, and knee as the femoral, sciatic, and obturator nerves course from the lumbar spine through the greater hip area. Several diagnostic tools can help discern a primary hip or spine pathology.
History
Patients with groin pain are seven times more likely to have symptomatic hip pathology regardless of presence of spine disease.10 Pain described as aching, especially when reproduced upon weight bearing, suggests mechanical OA-related pain from the hip. Alternatively, pain described as tingling, shock-like, or burning is more consistent with radiculopathy and is suggestive of lumbar pathology when accompanied by cutaneous sensory impairment in a dermatomal pattern.4
Physical Exam
Tests Suggesting a Primary Hip Pathology
Gait observation can strongly inform the differential diagnosis. Antalgic gait, with a shortened stance phase, suggests mechanical pelvic pain secondary to hip degeneration.11 Trendelenburg gait can be seen with either hip or spine pathology. With hip pathology this is due to abductor weakness and pain; with spine pathology this is due to L4-S1 myotome weakness. A limp, limited internal rotation or pain at the end of internal rotation suggests a primary hip pathology with or without a coexisting spine pathology.10 Groin pain is more associated with primary hip pathology.
Tests Suggesting a Primary Spine Pathology
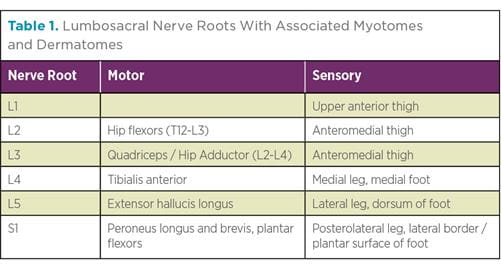
Physical exam findings are less sensitive for lumbar pathologies as they present with widely varying symptoms. Sensory, motor, and reflex deficiencies may be present in patients with lumbar radiculopathies, which can localize the affected nerve root (Table 1). Although a femoral tension sign is less than 20% sensitive to lumbar stenosis, a positive finding is five times more likely to be found in patients with lumbar stenosis than with an isolated hip pathology and indicates upper lumbar radiculopathy.10,12 A positive straight leg or contralateral straight leg is also consistent with a lower lumbar radiculopathy. Pain on extension in a forward bend test is consistent with lumbar stenosis or instability, and reproduction of pain on direct palpation of the lumbar vertebral column suggests a spine pathology.
Imaging and Injections
Local injections are often used to confirm symptom etiology in patients with HiSS after obtaining radiographic evidence of pathology. However, imaging should be correlated to physical exam findings since many patients with radiographic evidence of degeneration are asymptomatic.
Hip
Standard standing AP pelvis, cross-table lateral, and frog-leg radiographs can be used to evaluate the hip joint (e.g., Figure 1). CTs and AP radiographs can be used to assess alignment and positioning of either the native hip or arthroplasty components, including acetabular anteversion and inclination, femoral version and inclination, femoral offset, and leg-length discrepancy. Pain relief upon fluoroscopically guided hip injection in patients with radiographic OA suggests primary hip pathology, and incomplete or no pain relief suggests a lumbar pathology.1 Pain relief upon intra-articular bupivacaine injection was found to be 87% sensitive and 100% specific to a primary hip pathology.13
Spine
AP and lateral flexion-extension radiographs are first-line tests for suspected lumbar pathologies, and full-length lateral standing radiographs should be obtained to determine spinal curvature and spinopelvic sagittal balance (Figures 2 and 3). Lumbar spine MRIs are used to assess soft tissue and bony impingements, including nerve root and cord compression (Figure 4). Pain relief with an epidural steroid injection (ESI) suggests a primary spinal pathology. However, patients for whom ESIs have not provided pain relief may improve following lumbar decompression,12 so a negative response to ESI should not exclude the lumbar spine as the underlying cause of symptoms.
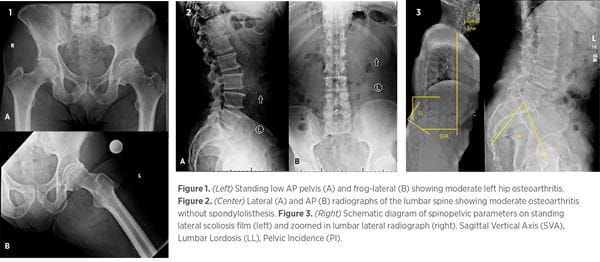
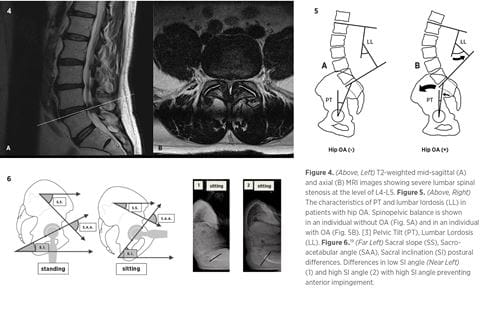
Figures 1, 2, and 4 represent clinical radiographs from the same patient. Their clinical presentation is left-sided low back, buttock, hip, and groin pain without clear radicular pathology. So, is it the hip or the spine, or both?
Misdiagnosis or inappropriately characterized HiSS can range in consequences from simply continued symptoms of pain and discomfort to extraneous surgical procedures with failed outcomes, complications, and subsequent reoperations. Compensatory changes that occur secondary to altered spinopelvic parameters following a hip or spine surgery can be a source of continued pain and complication.
Following total hip arthroplasty (THA), patients with lumbar spine disease (lumbosacral spondylosis, lumbar disk herniation, acquired spondylolisthesis, and degenerative disk disease) experience a significant increase in risk for complication, with prosthetic hip dislocation the most common.5,14
Patients with prior spinal fusion had significantly higher rates of complications, including dislocation revision, loosening, and any prosthetic-related complication within 24 months.15-17 Interestingly, when treating concomitant hip and spine pathologies, THA before spinal fusion is associated with decreased rates of hip dislocation and revision surgeries when compared to spinal fusion before THA, providing evidence of an optimized chronology.18
Patients with a previous lumbar fusion, particularly extending to the pelvis, jeopardize their spinopelvic accommodation, the ability of the pelvis to allow the increased motion required of change in posture.19 Sacral slope and pelvic tilt are critical in defining the range of spinopelvic accommodation, which when reduced in association with increased lumbar lordosis can lead to posterior hip instability (Figures 4-6).20
Specifically, a flexion deformity of the hip causes the pelvis to rotate anteriorly and develop compensatory hyperlordosis of the lumbar spine.3 Correcting this hyperlordosis may decrease the anterior acetabular coverage, ultimately accelerating degeneration of the hip.3 Compensatory hyperlordosis of the lumbar spine can result in foraminal stenosis and radicular symptoms.2,4 These altered spinopelvic kinematics impact the range of acetabular positioning with decreased pelvic tilt causing acetabular retroversion, while increased pelvic tilt causes acetabular anteversion, either of which increases risk for dislocation.4
The impact of THA on spinopelvic alignment parameters has been shown to reduce not only hip pain but also low back pain.21-24 In patients receiving a hip arthroplasty for OA with low back pain prior to surgery, symptom reduction is linked to improved spinopelvic parameters and corrected femoral neck anteversion of the arthritic hip.22,23 Two-thirds of patients who present with coexisting hip and spine pathologies with lumbar pain have reduced pain following THA, with half of the original patient population having known spine disorders.21
Several studies have investigated the mechanisms in which lumbar spine pathology affects the hip; however, limited literature exists describing the mechanism by which hip pathology impacts the spine.25,26 Furthermore, these studies do not investigate active, dynamic patient kinematics, which is crucial to understanding the relationship between the hip and spine in HiSS.
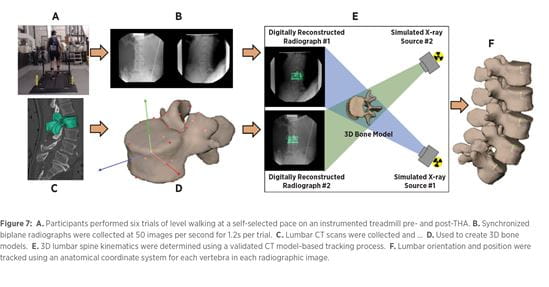
Current prospective work at the University of Pittsburgh Department of Orthopaedic Surgery Biodynamics Laboratory (BDL) seeks to better describe the dynamic relationship of these coordinated joint pathologies. Specifically, investigators are studying changes in lumbar kinematics that lead to the resolution of low back pain following total hip arthroplasty. This study involves using a custom volumetric-based bone model tracking system to monitor three-dimensional bone kinematics throughout the full gait cycle.27-32 Using biplane radiography, lumbar images are recorded while subjects walk at a self-selected pace. This data, along with a CT scan, are used to complete a 3D skeletal reconstruction of dynamic motion27 (Figure 7). Trials are completed pre- and post-THA to quantify dynamic lumbar kinematic changes while walking, since many patients suffer pain while upright and walking. This study also hopes to identify static and kinematic diagnostic parameters to predict low back pain resolution in patients receiving THA. With results from this study, the BDL aims to aid clinical diagnosis and therapeutic decision-making in patients with HiSS.
Authors
Spencer E. Talentino, BS
MS II, University of Pittsburgh School of Medicine
Tom W. Evashwick-Rogler, MS
MS II, University of Pittsburgh School of Medicine
Richard Wawrose, MD
Resident Physician, Department of Orthopaedic Surgery, University of Pittsburgh School of Medicine
Michael O’Malley, MD
Assistant Professor, Department of Orthopaedic Surgery, University of Pittsburgh School of Medicine, Division of Arthroplasty
Jeremy D. Shaw MD, MS
Assistant Professor, Department of Orthopaedic Surgery, University of Pittsburgh School of Medicine, Division of Spinal Surgery
1 Devin CJ, et al. Hip-spine Syndrome. J Am Acad Orthop Surg. 2012; 20(7): 434-442.
2 Offierski CM, MacNab I. Hip-spine Syndrome. Spine (Phila Pa 1976). 1983; 8(3): 316-21.
3 Okuzu Y, et al. Hip-Spine Syndrome: Acetabular Anteversion Angle Is Associated With Anterior Pelvic Tilt and Lumbar Hyperlordosis in Patients With Acetabular Dysplasia: A Retrospective Study. JB JS Open Access. 2019; 4(1): e0025.
4 Buckland AJ, et al. Differentiating Hip Pathology From Lumbar Spine Pathology: Key Points of Evaluation and Management. J Am Acad Orthop Surg. 2017; 25(2): e23-e34.
5 Prather H, van Dillen L. Links Between the Hip and the Lumbar Spine (Hip Spine Syndrome) as They Relate to Clinical Decision Making for Patients With Lumbopelvic Pain. PM&R. 2019; 11(S1): S64-S72.
6 Kalichman L, et al. Spinal Stenosis Prevalence and Association With Symptoms: The Framingham Study. Spine J. 2009; 9(7): 545-550.
7 Strand V, et al. Prevalence of Axial Spondyloarthritis in United States Rheumatology Practices: Assessment of Spondyloarthritis International Society Criteria Versus Rheumatology Expert Clinical Diagnosis. Arthritis Care Res (Hoboken). 2013; 65(8): 1299-1306.
8 Jordan JM, et al. Prevalence of Hip Symptoms and Radiographic and Symptomatic Hip Osteoarthritis in African Americans and Caucasians: The Johnston County Osteoarthritis Project. J Rheumatol. 2009; 36(4): 809-815.
9 Lawrence RC, et al. Estimates of the Prevalence of Arthritis and Other Rheumatic Conditions in the United States. Part II. Arthritis Rheum. 2008; 58(1): 26-35.
10 Brown MD, et al. Differential Diagnosis of Hip Disease Versus Spine Disease. Clin Orthop Relat Res. 2004; (419): 280-284.
11 DeFroda SF, Daniels AH, Deren ME. Differentiating Radiculopathy From Lower Extremity Arthropathy. Am J Med. 2016; 129(10): 1124.e1-7.
12 Weinstein JN, et al. Surgical Compared With Nonoperative Treatment for Lumbar Degenerative Spondylolisthesis. Four-Year Results in the Spine Patient Outcomes Research Trial (SPORT) Randomized and Observational Cohorts. J Bone Joint Surg Am. 2009; 91(6): 1295-1304.
13 Kleiner JB, Thorne RP, Curd JG. The Value of Bupivicaine Hip Injection in the Differentiation of Coxarthrosis From Lower Extremity Neuropathy. J Rheumatol. 1991; 18(3): 422-427.
14 Blizzard DJ, et al. The Impact of Lumbar Spine Disease and Deformity on Total Hip Arthroplasty Outcomes. Orthopedics. 2017; 40(3): e520-e525.
15 Barry JJ, et al. Early Outcomes of Primary Total Hip Arthroplasty After Prior Lumbar Spinal Fusion. J Arthroplasty. 2017; 32(2): 470-474.
16 Phan D, Bederman SS, Schwarzkopf R. The Influence of Sagittal Spinal Deformity on Anteversion of the Acetabular Component in Total Hip Arthroplasty. Bone Joint J. 2015; 97-b(8): 1017-1023.
17 York PJ, et al. The Relationship of Pelvic Incidence to Post-Operative Total Hip Arthroplasty Dislocation in Patients With Lumbar Fusion. Int Orthop. 2018; 42(10): 2301-2306.
18 Malkani AL, et al. Does Timing of Primary Total Hip Arthroplasty Prior to or After Lumbar Spine Fusion Have an Effect on Dislocation and Revision Rates? J Arthroplasty. 2019; 34(5): 907-911.
19 Lazennec JY, Brusson A, Rousseau MA. Lumbar-pelvic-femoral Balance on Sitting and Standing Lateral Radiographs. Orthop Traumatol Surg Res. 2013; 99(1 Suppl): S87-103.
20 Mudrick CA, Melvin JS, Springer BD. Late Posterior Hip Instability After Lumbar Spinopelvic Fusion. Arthroplast Today. 2015; 1(2): 25-29.
21 Parvizi J, et al. Back Pain and Total Hip Arthroplasty: A Prospective Natural History Study. Clin Orthop Relat Res. 2010; 468(5): 1325-1330.
22 Piazzolla A, et al. Spinopelvic Parameter Changes and Low Back Pain Improvement Due to Femoral Neck Anteversion in Patients With Severe Unilateral Primary Hip Osteoarthritis Undergoing Total Hip Replacement. Eur Spine J. 2018; 27(1): 125-134.
23 Weng W, et al. The Effect of Total Hip Arthroplasty on Sagittal Spinal-Pelvic-Leg Alignment and Low Back Pain in Patients With Severe Hip Osteoarthritis. Eur Spine J. 2016; 25(11): 3608-3614.
24 Ben-Galim P, et al. Hip-spine Syndrome: The Effect of Total Hip Replacement Surgery on Low Back Pain in Severe Osteoarthritis of the Hip. Spine (Phila Pa 1976). 2007; 32(19): 2099-2102.
25 Shum GL, Crosbie J, Lee RY. Effect of Low Back Pain on the Kinematics and Joint Coordination of the Lumbar Spine and Hip During Sit-To-Stand and Stand-To-Sit. Spine (Phila Pa 1976). 2005; 30(17): 1998-2004.
26 Igawa T, et al. Kinetic and Kinematic Variables Affecting Trunk Flexion During Level Walking in Patients With Lumbar Spinal Stenosis. PLoS One. 2018; 13(5): e0197228.
27 Dombrowski ME, et al. ISSLS PRIZE IN BIOENGINEERING SCIENCE 2018: Dynamic Imaging of Degenerative Spondylolisthesis Reveals Mid-Range Dynamic Lumbar Instability Not Evident on Static Clinical Radiographs. Eur Spine J. 2018; 27(4): 752-762.
28 Aiyangar A, et al. Apportionment of Lumbar L2-S1 Rotation Across Individual Motion Segments During a Dynamic Lifting Task. J Biomech. 2015; 48(13): 3709-3715.
29 Aiyangar A, et al. Instantaneous Centers of Rotation for Lumbar Segmental Extension In Vivo. J Biomech. 2017; 52: 113-121.
30 Aiyangar AK, et al. Capturing Three-dimensional In Vivo Lumbar Intervertebral Joint Kinematics Using Dynamic Stereo-X-ray Imaging. J Biomech Eng. 2014; 136(1): 011004.
31 Anderst WJ, Vaidya R, Tashman S. A Technique to Measure Three-Dimensional In Vivo Rotation of Fused and Adjacent Lumbar Vertebrae. Spine J. 2008; 8(6): 991-997.
32 Diebo BG, et al. Radiographic Categorization of the Hip-spine Syndrome in the Setting of Hip Osteoarthritis and Sagittal Spinal Malalignment. J Am Acad Orthop Surg. 2019; 27(17): 659-666.