Password Reset
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Experts from the UPMC Heart and Vascular Institute, UPMC Department of Cardiothoracic Surgery, and UPMC Department of Surgery recently published new research regarding donation after circulatory death (DCD) in The Journal of Thoracic and Cardiovascular Surgery.
Nicholas Hess, MD, was first author of the study with Yeahwa Hong, MD, Pyongsoo Yoon, MD, Johannes Bonatti, MD, Ibrahim Sultan, MD, Derek Serna-Gallegos, MD, Danny Chu, MD, Gavin Hickey, MD, Mary Keebler, MD, and David Kaczorowski, MD, collaborating as part of the research team.
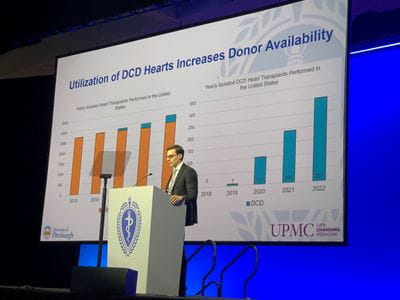

Nick Hess, MD, presenting this data at a Plenary Session at the AATS meeting in Los Angeles. UPMC Team Preparing DCD Heart.
The goal of this study was to assess the performance of DCD hearts for both waitlist and post-transplant outcomes in the United States. UPMC experts reviewed the United Network for Organ Sharing (UNOS) database to identify all adult waitlisted and transplanted candidates between October 18, 2018, and December 31, 2022.
In total, 14,803 candidates were waitlisted. The waitlisted candidates were grouped into cohorts depending on whether they had been approved for donation after brain death (DBD) offers only or also approved for DCD offers. 12,287 of the candidates were approved for DBD donors only and 2,516 approved for DCD donors.
12,238 recipients ended up receiving a transplant: 11,636 with DBD hearts and 602 with DCD hearts. Median waitlist times were significantly shorter for those receiving DCD hearts. Transplantation was then compared between both cohorts through a post-transplant analysis. One-year post-transplant survival was compared between unmatched and propensity-score-matched cohorts of DBD and DCD recipients.
Importantly, results showed that one-year post-transplant survival was similar between unmatched and propensity score–matched cohorts of DBD and DCD recipients.
Ultimately, the use of DCD hearts allows for a higher probability of transplantation and a lower incidence of death or deterioration while on the waitlist. Therefore, this data is evidence that DCD hearts can be safely used to reduce waitlist times and achieve post-transplant survival outcomes that are equivalent to those using hearts from standard brain-dead donors.
"Data from this study demonstrates that we can safely increase the availability of donor hearts for our patients in need of a heart transplant by using DCD donors," says Dr. Kaczorowski, Surgical Director of the Advanced Heart Failure Center at UPMC and senior author on the study. "Utilizing DCD donors has had a positive impact on our clinical heart transplant program here at UPMC by making more hearts available for patients in need."
Reference
Nicholas R. Hess, Yeahwa Hong, Pyongsoo Yoon, Johannes Bonatti, Ibrahim Sultan, Derek Serna-Gallegos, Danny Chu, Gavin W. Hickey, Mary E. Keebler, David J. Kaczorowski, Donation after circulatory death improves probability of heart transplantation in waitlisted candidates and results in post-transplant outcomes similar to those achieved with brain dead donors, The Journal of Thoracic and Cardiovascular Surgery, 2023, ISSN 0022-5223, https://doi.org/10.1016/j.jtcvs.2023.09.012.