Password Reset
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
Forgot your password? Enter the email address you used to create your account to initiate a password reset.
A number of new initiatives, research projects, and program updates have occurred in recent years on the audiology front in the Department of Otolaryngology.
Catherine V. Palmer, PhD, director of the UPMC Center for Audiology and Hearing Aids, describes much of the current work as fitting under the theme of interventional audiology (IA), which primarily involves treating hearing loss when it is not the primary concern of the patient, but the untreated hearing loss will negatively impact the health outcome that is of concern.

“This is a new approach and not widely adopted at this time in the field, but there is a growing interest in it as centers like ours have begun to publish data on the impact of interventional audiology. IA takes audiologists out of the clinic to where patients need them. It relies on audiologists overseeing these programs but often using assistants to provide the workforce at this level. It is a model that is showing many benefits,” says Dr. Palmer.
Dr. Palmer is an associate professor in both the Department of Communication Science and Disorders and the Department of Otolaryngology. She serves as the Director of Audiology for the UPMC Health System. Dr. Palmer conducts research in the areas of auditory learning post-hearing aid fitting, the relationship between hearing and cognitive health, and matching technology to individual needs.
She has published more than 90 articles and book chapters on these topic areas, as well as provided more than 100 national and international presentations. Dr. Palmer is the Director of the AuD program at the University of Pittsburgh and teaches the graduate level amplification courses. She serves as Editor-in-Chief of Seminars in Hearing and currently is President-Elect
for the American Academy of Audiology.
Dr. Palmer has been awarded the Editor’s Award for the American Journal of Audiology, the Dean’s Distinguished Teaching Award SHRS, the University of Pittsburgh Provost’s Award for Excellence in Mentoring, and the Pennsylvania Academy of Audiology Award for Outstanding Service.
This program involves having an audiologist in each of 33 UPMC senior living facilities (independent living, assisted living, and skilled nursing and rehabilitation facilities) once per month.
In addition, the program has a “Communication Facilitator” in one of the assisted living facilities who is there to ensure that everyone can communicate day-to-day. This aspect of the program is a new model undergoing testing and evaluation.
The program involves various activities, including caring for hearing aids, using assistive devices (phone devices, TV devices), ensuring common rooms are equipped with listening devices, and other interventions.
“We received funding from the Hearst Foundation to begin and test this program for its first year, and we are now applying for PCORI funding to test these intervention models on a broader scale,” says Dr. Palmer.
In 2017, Dr. Palmer and colleagues published initial findings of their pilot program in the journal Seminars in Hearing, where they outline the key components of this communication assistance program and innovative model for delivering audiology services to a diverse group of older adults in multiple residential living and care settings.

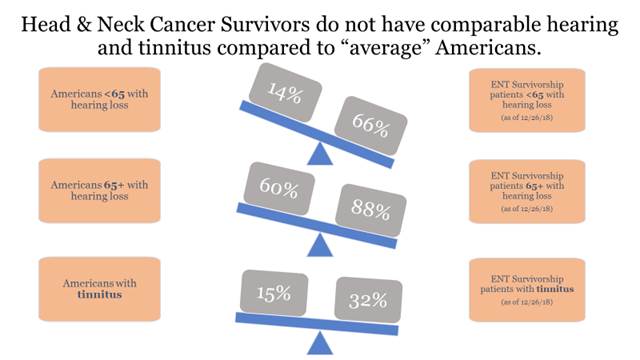
With the high incidence of hearing loss and tinnitus affecting patients treated for head and neck cancer, either as a result of surgical procedures or from the side effects of chemotherapy and radiation treatments, managing patients’ hearing health and audiology concerns are important aspects of their overall post-treatment care plan. Dr. Palmer’s Center has an embedded audiologist assigned to work within the HNC Survivorship Clinic for this very purpose.
“Every HNC survivor patient has their hearing screened on the day of their first visit. If they fail the screening, they are provided with a simple amplifier so they can fully participate in their extended appointment in the clinic where they will be seeing and communicating with multiple professionals. The first visit is such an important time for these individuals. We want them to fully understand and hear everything being said, and we also want them to know exactly how vested we are in their overall health. This aspect of our approach has met with a great deal of success and positive feedback since the clinic first started in 2016,” says Dr. Palmer.
Patients who fail the initial hearing screening also are offered a full audio evaluation the same day to help put them onto a pathway to hearing health care at the outset. Dr. Johnson has been interested particularly in the prevalence of hearing loss in these HNC survivors.
“These individuals experience hearing loss and tinnitus at a higher rate than the general population. Physicians treating individuals for head and neck cancer with chemotherapy or radiation should be connecting them as early as possible to audiology, so the patient will know what options exist in managing these side effects. There are data to indicate that the majority of individuals are not referred to audiology. This would be a simple practice change for most ENT physicians given the proximity of audiology services and one that could significantly improve HNC survivors’ quality of life and overall hearing health,” says Dr. Palmer.
These same services are provided in the UPMC Trauma Outpatient clinic, which is another example of a clinic where individuals see a number of health care providers in one day and access to communication through improved hearing is essential to support full participation.